Anatomical and physiological principles
To understand the specific anatomical differences between tracheotomy (incision of the trachea) and laryngectomy (removal of the larynx), it is of particular importance to first visualise and correctly understand the airways of a healthy person.
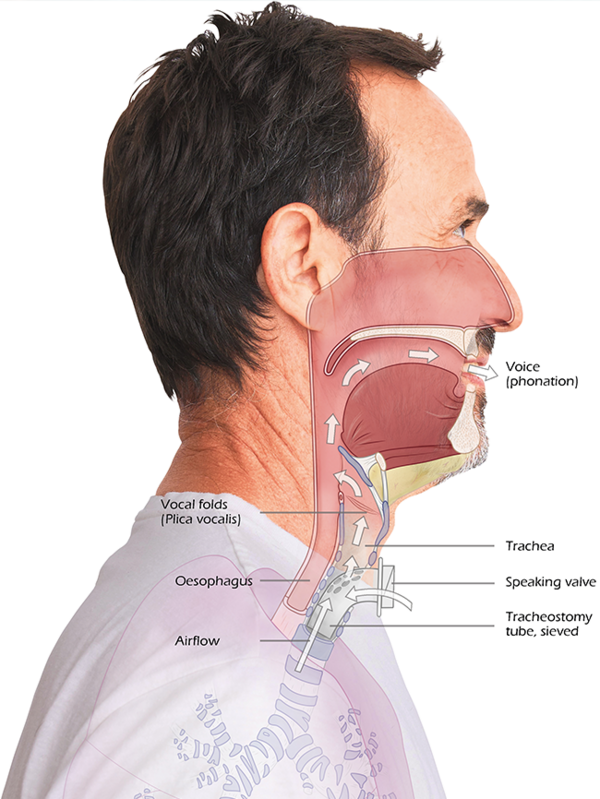
The schematic illustrations show that the trachea and oesophagus run in close proximity to each other, with the oesophagus positioned behind the trachea. The larynx forms an important interface between these two structures. It not only takes over the function of the voice, but also the correct direction of air and food as well as protection against swallowing the wrong way by closing the trachea with the epiglottis as needed during the process of swallowing. Inhalation and exhalation in a healthy person can be performed via the nose as well as via the mouth. Therefore, if the nose is occluded, respiratory function can still be adequately maintained exclusively via the mouth.
Different diseases such as acute deterioration of the respiratory situation up to requiring ventilation, severe tumorous events in the respiratory tract or neurological diseases make the creation of a tracheotomy, i.e. performing a tracheotomy or even the removal of the larynx - the laryngectomy - necessary.
In all cases, there are specific changes to the anatomy which cause fundamental consequences for the respiratory situation of the affected person.

Before Tracheotomy
- Larynx present
- Oesophagus and trachea intact
- Interface larynx
- Phonation/Direction/Protection
- Breathing via the mouth, nose throat area
After Tracheotomy
- Preserved larynx
- Opened trachea
- Breathing via tracheostoma, poss. nose
- Displacement of airway by tracheostoma, may be reversible
What is a Tracheotomy?
A tracheotomy becomes necessary to secure the patient's respiratory situation. This may prove necessary in the context of complex surgery in the facial region, due to an emergency situation or also in the case of foreseeable long-term ventilation requirements.
During a tracheotomy, the front wall of the windpipe (trachea) is opened to create direct access to the lower respiratory tract.
Different placement techniques are used depending on the diagnosis and must later be taken into account in the subsequent provision of aids and patient care. As a result of the tracheotomy, both inhalation and exhalation are performed via the tracheostoma.
The newly created airway bypasses the larynx, which means that no voice can be produced initially.
Special combinations of aids, such as the tracheostomy tube with a speaking valve, can in most cases reactivate the voice function at a later stage of treatment.
Tracheotomy or tracheostomy
In Anglo-American countries in particular, the terms "tracheostomy" or "tracheotomy" are used for the same procedure - the tracheotomy. Elsewhere, the distinction between tracheotomy for the incision and tracheostomy for the creation of an epithelialised tracheostoma has become established.
For the patient, the change in dead space (portion of the airway not available for gaseous exchange) after tracheostomy is immediately noticeable at the first breath by a significant reduction in breathing resistance.
Although this effect is initially perceived as positive, it is counterproductive for physiological reasons, because breathing resistance is important for maintaining lung volume and function. Tracheostomy tubes increase resistance, particularly in combination with an HME (Heat and Moisture Exchanger).

The benefits of a tracheotomy
The use of a tracheal tube for ventilation should be changed as soon as possible to a tracheotomy with a well-fitted tracheostomy tube to protect the larynx and vocal cords.
This makes it easier to perform oral care and improves communication skills and oral food intake. The tracheotomy itself offers both active benefits (safe airway, good acceptance of the tracheostomy tube, reduced foreign body sensation, high fixation security, efficient bronchial toilette) as well as passive benefits (fewer sedatives, improved oral care, rapid oralisation, early mobilisation) in different ways.
Classic indications for the placement of a tracheostoma are found in very differing medical situations.
- Mechanical airway obstruction (oedema, tumours, injuries, chemical burns, foreign bodies)
- Internal incidents (cardiological, pulmonological)
- Neurological diseases, dysphagia and aspiration risks
- Long-term ventilation/weaning
Complications
Various complications are possible in the course of a tracheostomy and it is imperative to keep these in mind. In general, bleeding, infection and granulation can cause problems at any time. Notable complications include: incorrect placement of the cannula, pressure ulcers in the area of the cannula tip, pneumothorax formation, tracheal wall damage due to cuff pressure errors, oesophageal fistula formation, scars and stenoses in the trachea.





